Meet the zygote
Read more
Find out what zygotes are, what they do and how MitoQ might be able to support their health.
Calculated at checkout
$0.00 USD
Find out what zygotes are, what they do and how MitoQ might be able to support their health.
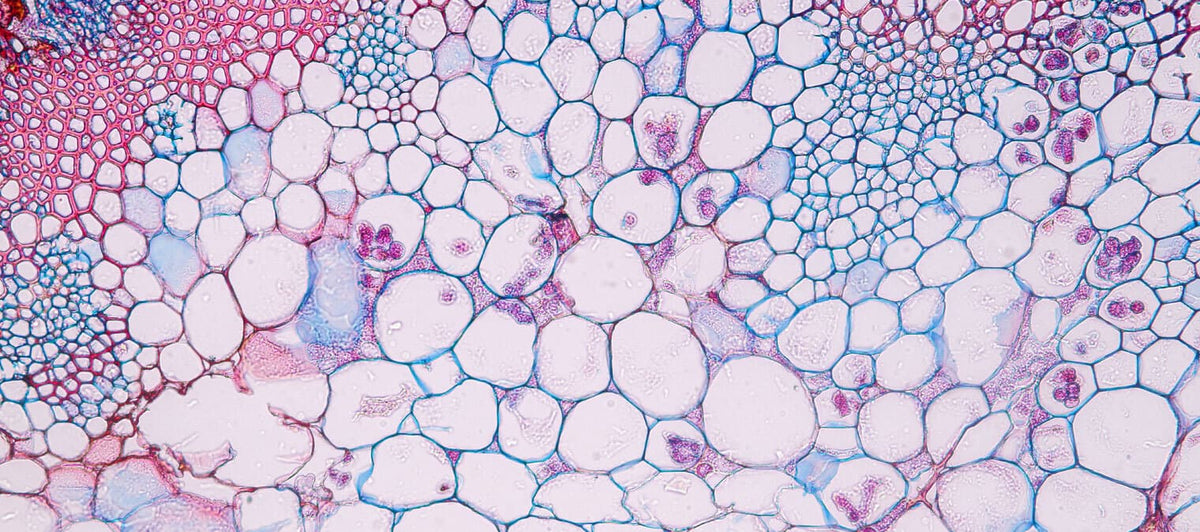
One of the greatest wonders in biology is the ability of the female egg to grow into an entire human being. The zygote stage is where the long process of growing a new human (or any new sexually reproduced plant, animal, fungus or protist, for that matter) begins. In this article, we’ll dive into how a zygote is formed, the difference between a zygote vs embryo and discuss cell health.
A zygote is a fertilized egg. A zygote only exists for a brief period once a sperm cell has reached and fused with the egg - but before an embryo is formed; hence it can also be thought of as the sperm-egg complex.
Interestingly, the female egg (oocyte) contains pretty much everything needed for life. In fact, female eggs are essentially halfway to becoming a zygote every time ovulation (the period where a female human produces an egg, approximately once every month) occurs. During ovulation, an egg cell grows and matures, busily producing new proteins, deactivating other proteins, reshuffling its mitochondria, and generally preparing cell materials for possible fertilization by sperm. The egg cell also undergoes the first phase of meiosis.
Meiosis: A type of cell division that only occurs when creating reproductive cells (eggs and sperm). In the rest of our body, cells divide and grow constantly too but they all have the same DNA. In meiosis, the DNA is mixed and swapped so that all the resulting cells produced are totally independent and unique from one another and from the parent cell. Meiosis is split into two phases: the first happens in male sperm production or female egg production, while the second phase happens during fertilization. It is thanks to meiosis that you could have 20 children, and yet they would all be genetically different from each other, you, and your partner!
During sexual reproduction, sperm is deposited into the vagina in the range of around two to five million sperm cells. That may seem like an excessive amount, but sperm cells lack the machinery to be able to repair themselves, so it’s a tradeoff with quantity; there is a connection between a greater number of sperm cells and a higher chance of fertilization. The body only has so much energy and resources it can contribute to the costs of reproduction, so we can think of it economically: in theory, sperm fall under the "cheap and small” reproductive strategy, meaning the body can make lots of them but they can die easily, whereas egg cells fall under the “expensive and large” strategy, with the body investing in complexity over quantity. Still, it remains a mystery why there is such a huge redundancy in the number of sperm cells released and egg cells unused over the human reproductive lifespan.
As opposed to common myths about fertilization, sperm do not dash to the egg in an Olympic style swimming race competition – it's more like they lope over the finish line after a long, challenging obstacle course, with the organizers of the obstacle course (otherwise known as the female reproductive tract) cheering them on!
Once inside the vaginal canal, sperm cells can survive longer than scientists originally thought. That is because sperm can be stored for days in pockets of the cervix lining known as crypts that provide a reservoir for sperm before they’re either transferred or disposed of. This storage of sperm – and the number of crypts available – is enhanced by the hormone estrogen in the female. Furthermore, unlike the ‘swimming race’ theory, evidence suggests that sperm cells move along the female tract passively, with the uterus pumping sperm cells up until the exit of the uterine cavity. The moment when sperm cells exit the uterine cavity and reach the entrance to the fallopian tube is where sperm motility becomes important, as they now actively head towards the oocyte. They may not necessarily travel in a straight line, and it remains unknown exactly if and how there is chemical attraction involved in sperm cells seeking out the egg. The female egg cell also travels upward from the ovary into the fallopian tubes, helped by contractions of the fallopian tube and pushed along by little cell hairs known as cilia.
Sperm cells gradually die off the further along the female tract they go, as they can be killed by the acidic conditions, trapped by the mucus of the cervix, lost in crypts, off-track down the wrong fallopian tube (it’s a 50/50 gamble on which one will contain the egg), or they die due to physical abnormalities like a misshapen head or tail. Few sperm make it into the uterus, and fewer still into the fallopian tube. Cells in the inner lining of the fallopian tube appear to bind sperm cells and preferentially allow only higher quality sperm cells to continue on to pass a layer of follicle cells and reach the protective protein layer (zona pellucida) surrounding the egg. Once a sperm cell gets through the zona pellucida, it becomes an impenetrable barrier in order to seal other sperm out. If too many sperm cells happen to arrive at the egg at the exact same time, the egg will not survive, or it may accumulate genetic abnormalities. That is a consideration that has to be taken into account during in vitro fertilization methods. Hence the female reproductive tract has evolved this biological obstacle course for a reason: to limit the number of sperm cells surrounding the egg.
If a sperm cell does arrive, it fuses with the egg in the fallopian tube (not in the ovaries, as many people may expect) and signals phase two of meiosis to proceed in the egg, kickstarting its transformation to a zygote. The DNA from the sperm and egg is fused during meiosis to create a zygote that is genetically unique from either parent, with the sex likely determined by whether the sperm cell happens to be carrying an X or Y chromosome to pair with the X chromosome in the egg to make a female (XX) or male (XY). In every single species that has been studied so far, this moment of sperm-egg fusion is accompanied by a burst of calcium and a flash of light caused by zinc sparks. In mammals, these calcium bursts occur in waves over several hours that complete egg activation.
If no sperm cell ever arrives, the egg is discarded via menstruation. It’s kind of like a cellular melodramatic romance: both the egg and the sperm are on a ticking clock, destined to die unless they find each other.
The zygote’s main prerogative is to grow and develop into an embryo.
Every human on the planet started off as one individual cell, a zygote, containing a full set of DNA – that is, 23 chromosomes from the female, and 23 chromosomes from the male. This DNA is like a set of instructions, so that when the zygote begins the journey of creating a new human, it has all the blueprint necessary to construct every cell. The unique genetic combination that the zygote inherits from the mother and father now becomes the genetic programming all of the subsequent cells will have as the zygote becomes an embryo.
The zygote grows, copies its DNA, then splits into two identical cells. It repeats this process, doubling its cell number over and over again while it journeys through the female reproductive tract. Approximately 30-70% of conceptions fail the first month of pregnancy.
Week 1 of pregnancy is counted from the first day of the last period in a female’s menstrual cycle, rather than from the first day of fertilization. Hence fertilization technically takes place in week 3 of pregnancy – despite the female not actually being pregnant up until that point.
The zygote begins dividing within a matter of hours after fertilization takes place and begins its journey down the fallopian tubes toward the uterus, which will take several days to complete. Initially, the zygote divides into about 12-15 identical cells in a big cellular ball known as a morula, then and after five or six days, it grows into a bigger ball of cells known as a blastocyst, roughly a fifth of the size of this full stop.
Eventually this blastocyst reaches the uterus, where it burrows and implants itself into the lining. At the point the blastocyst has implanted itself, someone is considered pregnant. The body begins to produce the human chorionic gonadotropin (hCG) hormone, which can be detected by home pregnancy tests or blood tests. Once the blastocyst is implanted, another stage of cell division takes place where half of the blastocyst becomes an embryo while the other half develops into a placenta to provide nourishment. The uterus wall is thick during ovulation and helps the blastocyst ‘stick’ (hence why many contraception methods work to stop an embryo implanting into the uterine wall).
The journey from zygote to embryo is officially complete. All in all, it took about two weeks for the zygote to become an embryo, otherwise known as week 5 of pregnancy. From about week 10 of pregnancy, the embryo is referred to as a fetus.
Evidence has pointed to a link between mitochondrial function and fertility including sperm motility and egg health, and a developing zygote depends on a pool of mitochondria to power growth all the way through key events in fertilization and embryonic development.
Did you know: Mitochondria have their own type of DNA separate to the rest of your cells – mitochondrial DNA - which is passed only through the maternal line. That means you have the mitochondrial DNA of your mother, and grandmother, and great-grandmother, all the way back to the dawn of humanity.
Whilst there are promising results in this area, it is important to note that we do not recommend MitoQ for pregnant women or as a fertility strategy. Whilst it has an excellent safety profile, MitoQ has not been specifically studied in human pregnancy. We emphasize that these insights are simply interesting findings originating from preliminary, independent research, shared for educational purposes. We do not claim MitoQ will have any benefits for fecundity.
Everything starts inside a cell – and it all ties back to the time you were just a zygote, with a whole lot of potential. We’re simply fascinated by the role of mitochondria and cell health in reproduction and look forward to seeing further research in this exciting space.

MitoQ on The Balancing Act. Read the full interview here.
Dec 10, 2025 |4 mins to read

Dr. Mitchell and Dr. Balduzzi dive deep into the science of mitochondria - the tiny powerhouses inside your cells. Read the highlights.
Dec 9, 2025 |3 mins to read